A strong fall COVID booster campaign could save about 90,000 people living in the U.S. from dying of the virus and avoid more than 936,000 hospitalizations, according to a new study by the Commonwealth Fund.
As immunity wanes and new variants that can evade protection from early vaccines emerge, surges in hospitalizations and deaths are increasingly likely this fall and winter, the authors wrote. That makes it important that people get the bivalent boosters recently authorized by the Food and Drug Administration and help stop transmission, they wrote.
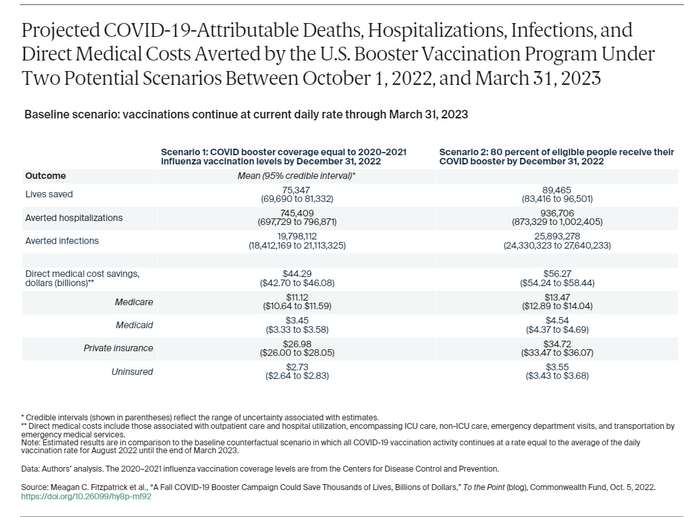
Researchers analyzed three scenarios to evaluate the impact of vaccination on reducing fatalities, hospitalizations and medical costs to both the Medicare and Medicaid programs.
The first measured the outcome if daily vaccination rates remain unchanged from current levels, where they have gradually declined since the first wave of the omicron variant. Federal financial support has also not been replenished, partly because of the perception among many Americans that the pandemic is over.
As of Oct. 3, some 68% of the U.S. population has had primary shots, but fewer than half of those have received a booster dose, and only 36% of those aged 50 and older have had a second booster.
The second and third scenarios looked at outcomes if rates increased by the end of 2022.
In the first scenario, researchers imagined booster uptake would track flu shot coverage in 2020 to 2021. The second assumed 80% of eligible individuals aged 5 and older get a booster by the end of 2022.
Source: Commonwealth Fund
The data found that more than 75,000 deaths could be prevented along with more than 745,000 hospitalizations if coverage reaches similar levels to 2021 to 2022 flu vaccination. The best scenario would save $56 billion in direct medical costs over the course of the next six months.
“Stratifying by insurance type, we found direct medical costs would be reduced by $11 billion for Medicare alone under scenario 1 and $13 billion under scenario 2,” the authors wrote. “An additional $3.5 to $4.5 billion in savings would accrue to Medicaid. Even if the federal government paid all vaccination costs, accelerated campaigns would generate more than $10 billion in net savings from federal programs like Medicare and Medicaid.”
The study comes as U.S. known cases of COVID are continuing to ease and now stand at their lowest level since late April, although the true tally is likely higher given how many people are testing at home, where the data are not being collected.
The daily average for new cases stood at 44,484 on Tuesday, according to a New York Times tracker, down 22% from two weeks ago. Cases are rising in most Northeastern states by 10% of more, while cases in the West are rising in Montana, Washington and Oregon.
The daily average for hospitalizations was down 12% at 27,334, while the daily average for deaths is down 8% to 393.
Coronavirus Update: MarketWatch’s daily roundup has been curating and reporting all the latest developments every weekday since the coronavirus pandemic began
Other COVID-19 news you should know about:
• Long COVID, a condition which can encompass symptoms such as respiratory distress, cough, “brain fog,” fatigue, and malaise, that last 12 weeks or longer after initial infection, is becoming a long term challenge as both employers and workers navigate an ever-mutating virus, according to Liz Seegert, writing for NextAvenue.org. The Centers for Disease Control and Prevention found that one in five COVID survivors younger than 65 experienced at least one incident that might be related to previous COVID-19 infection. Among those 65 and older, the rate was one in four. Their data also show that nearly three times as many people age 50 to 59 currently have long COVID than those 80 or older.
• A retired judge opened a public inquiry on Tuesday into how Britain handled the coronavirus pandemic, saying bereaved families and those who suffered would be at the heart of the proceedings, the Associated Press reported. Former Court of Appeal judge Heather Hallett said the inquiry would investigate the U.K.’s preparedness for a pandemic, how the government responded, and whether the “level of loss was inevitable or whether things could have been done better.”
• Health experts are keeping an eye on new versions of the BA.5 omicron subvariant amid concerns they can evade the drugs developed to fight COVID, Salon reported. Of particular concern are two named BQ.1 and BQ.1.1, along with BA.2.75.2 which is spreading in Singapore, India and parts of Europe. Then there’s XBB, which some research suggest is the most antibody-evasive strain tested so far.
• Eiger BioPharmaecuticals Inc.
EIGR,
said Wednesday it will not pursue emergency authorization of its experimental treatment for mild and moderate COVID-19 infections. It had asked the Food and Drug Administration to consider an EUA application based on data from the Together trial, a Phase 3 study that has assessed 11 possible treatments for COVID-19 that is being conducted in Brazil and Canada. Eiger said the FDA instead recommended the company consider running its own pivotal trial for peginterferon lambda that would support full approval of the drug.
Here’s what the numbers say:
The global tally of confirmed cases of COVID-19 topped 619.2 million on Wednesday, while the death toll rose above 6.55 million, according to data aggregated by Johns Hopkins University.
The U.S. leads the world with 96.5 million cases and 1,060,446 fatalities.
The Centers for Disease Control and Prevention’s tracker shows that 225.3 million people living in the U.S., equal to 67.9% of the total population, are fully vaccinated, meaning they have had their primary shots. Just 109.9 million have had a booster, equal to 48.8% of the vaccinated population, and 23.9 million of those who are eligible for a second booster have had one, equal to 36.6% of those who received a first booster.
Some 7.6 million people have had a shot of the new bivalent booster that targets the new omicron subvariants that have become dominant around the world.
